The YSRCCYP provides an invaluable and unique source of data that has been used for varied research as shown below
2024
The hidden barriers to using cancer registration data. Hughes, Nicola et al. The Lancet Oncology, Volume 25, Issue 11, 1390 - 1391
Sciberras P, Cromie K, Radford A, Glaser A, Feltbower RG, Hughes N. Survival Outcomes Following Chemotherapy for High-Grade Central Nervous System Tumors in Adolescents and Young Adults: An Exploration of Variations According to Ethnicity and Deprivation. J Adolesc Young Adult Oncol. 2024 Dec 5. doi: 10.1089/jayao.2024.0124. Epub ahead of print. PMID: 39636583.
Children were prospectively recruited to the Born in Bradford birth cohort between March 2007 and December 2010. Diagnoses of CHD were identified through linkage to the congenital anomaly register and independently verified by clinicians. Multivariable regression accounted for relevant confounders. Our primary outcome was the odds of 'below expected' attainment in maths, reading, and writing at ages 4-11 years.Educational records of 139 children with non-genetic CHD were compared with 11 188 age-matched children with no major congenital anomaly. Children with CHD had significantly higher odds of 'below expected' attainment in maths at age 4-5 years [odds ratio (OR) 1.64, 95% confidence interval (CI) 1.07-2.52], age 6-7 (OR 2.03, 95% CI 1.32-3.12), and age 10-11 (OR 2.28, 95% CI 1.01-5.14). Odds worsened with age, with similar results for reading and writing. The odds of receiving special educational needs support reduced with age for children with CHD relative to controls [age 4-5: OR 4.84 (2.06-11.40); age 6-7: OR 3.65 (2.41-5.53); age 10-11: OR 2.73 (1.84-4.06)]. Attainment was similar for children with and without exposure to cardio-pulmonary bypass. Lower attainment was strongly associated with the number of pre-school hospital admissions.
Cave DGW, Wands ZE, Cromie K, Hough A, Johnson K, Mon-Williams M, Bentham JR, Feltbower RG, Glaser AW. Educational attainment of children with congenital heart disease in the United Kingdom. Eur Heart J Qual Care Clin Outcomes. 2024 Aug 8;10(5):456-466. doi: 10.1093/ehjqcco/qcad068
Nicola F Hughes, Kirsten J Cromie, Richard G Feltbower, Martin G McCabe, Dan Stark. International Journal of Cancer. March 2024doi: 10.1002/ijc.34762.
Milner SH, Feltbower RG, Absolom KL, Glaser AW. Identifying social outcomes of importance for childhood cancer survivors: an e-Delphi study. J Patient Rep Outcomes. 2024 Feb 5;8(1):14. doi: 10.1186/s41687-023-00676-7
Design: Analysis of educational data linked to the ongoing Born in Bradford cohort study. Confounders were identified via causal inference methods and multivariable logistic regression performed.
Setting: Children born in Bradford Royal Infirmary (BRI), West Yorkshire.
Patients: All women planning to give birth at BRI and attending antenatal clinic from March 2007 to December 2010 were eligible. 12 453 women with 13 776 pregnancies (>80% of those attending) were recruited. Records of 555 children with major CA and 11 188 without were linked to primary education records.
Outcomes: Key Stage 1 (KS1) attainment at age 6–7 years in Maths, Reading, Writing and Science. SEN provision from age 4 to 7 years.
Results: 41% of children with major CA received SEN provision (compared with 14% without), and 48% performed below expected standards in at least one KS1 domain (compared with 29% without). The adjusted odds of children with CA receiving SEN provision and failing to achieve the expected standard at KS1 were, respectively, 4.30 (95% CI 3.49 to 5.31) and 3.06 (95% CI 2.47 to 3.79) times greater than their peers. Those with genetic, heart, neurological, urinary, gastrointestinal and limb anomalies had significantly poorer academic achievement.
Conclusions: These novel results demonstrate that poor educational attainment extends to children with urinary, limb and gastrointestinal CAs. We demonstrate the need for collaboration between health and education services to assess and support children with major CA, so every CA survivor can maximise their potential.
Wands ZE, Cave DGW, Cromie K, et al. Early educational attainment in children with major congenital anomaly in the UK. Archives of Disease in Childhood Jan 2024;109:326-333. doi: 109:326-333
Methods: We conducted a multicenter cohort study, recruiting 1114 TYA aged 13-24 years at diagnosis. Data collection involved a bespoke survey at 6,12,18, 24, and 36 months after diagnosis. Confounder adjusted analyses of perceived social support, illness perception, anxiety and depression, and health status, compared patients receiving NO-TYA-PTC care with those receiving ALL-TYA-PTC and SOME-TYA-PTC care. Results: Eight hundred and thirty completed the first survey. There was no difference in perceived social support, anxiety, or depression between the three categories of care. Significantly higher illness perception was observed in the ALL-TYA-PTC and SOME-TYA-PTC group compared to the NO-TYA-PTC group, (adjusted difference in mean (ADM) score on Brief Illness Perception scale 2.28 (95% confidence intervals [CI] 0.48-4.09) and 2.93 [1.27-4.59], respectively, p = 0.002). Similarly, health status was significantly better in the NO-TYA-PTC (ALL-TYA-PTC: ADM -0.011 [95%CI -0.046 to 0.024] and SOME-TYA-PTC: -0.054 [-0.086 to -0.023]; p = 0.006).
Conclusion: The reason for the difference in perceived health status is unclear. TYA who accessed a TYA-PTC (all or some care) had higher perceived illness. This may reflect greater education and promotion of self-care by health care professionals in TYA units.
Taylor RM, Whelan JS, Barber JA, Alvarez-Galvez J, Feltbower RG, Gibson F, Stark DP, Fern LA. The Impact of Specialist Care on Teenage and Young Adult Patient-Reported Outcomes in England: A BRIGHTLIGHT Study. J Adolesc Young Adult Oncol. 2024 Jun;13(3):492-501. doi: 10.1089/jayao.2023.0141. Epub 2024 Jan 30. doi: 10.1089/jayao.2023.0141
2023
Methods: Cancer registration data for 2674 children (0-14 years) in Yorkshire were analysed. Five-year survival estimates by ethnic group (south Asian/non-south Asian) and Townsend deprivation fifths (I-V) were compared over time (1997-2016) for leukaemia, lymphoma, central nervous system (CNS) and other solid tumours. Hazard ratios (HR: 95% CI) from adjusted Cox models quantified the joint effect of ethnicity and deprivation on mortality risk over time, framed through causal interpretation of the deprivation coefficient.
Results: Increasing deprivation was associated with significantly higher risk of death for children with leukaemia (1.11 (1.03-1.20)) and all cancers between 1997 and 2001. While we observed a trend towards reducing differences in survival over time in this group, a contrasting trend was observed for CNS tumours whereby sizeable variation in outcome remained for cases diagnosed until 2012. South Asian children with lymphoma had a 15% reduced chance of surviving at least 5 years compared to non-south Asian, across the study period.
Discussion: Even in the United Kingdom, with a universally accessible healthcare system, socio-economic and ethnic disparities in childhood cancer survival exist. Findings should inform where resources should be directed to provide all children with an equitable survival outcome following a cancer diagnosis.
K J Cromie, N F Hughes, S Milner, P Crump, J Grinfeld, A Jenkins, P D Norman, S V Picton, C A Stiller, D Yeomanson, A W Glaser, R G Feltbower. British Journal of Cancer. doi: 10.1038/s41416-023-02209-x
Methods: Young people currently aged between 16 and 25 years who had a cancer diagnosis before the age of 20 years and carers of a young person with cancer were invited to take part via social media and existing networks of service users. Data was collected during two interactive online workshops totalling 5 h and comprising of presentations from health data experts, case-studies and group discussions. With participant consent the workshops were recorded, transcribed verbatim and analysed using thematic analysis.
Results: Ten young people and six carers attended workshop one. Four young people and four carers returned for workshop two. Lack of awareness of how data is used, and negative media reporting were seen as the main causes of mistrust. Better communication and education on how data is used were felt to be important to improving public confidence. Participants want the ability to have control over their own data use. Late effects, social and education outcomes and research on rare tumours were described as key research priorities for data use.
Conclusions: In order to improve public and patient trust in our use of data for research, we need to improve communication about how data is used and the benefits that arise.
Hughes NF, Fern LA, Polanco A, Carrigan C, Feltbower RG, Gamble A, Connearn E, Lopez A, Bisci E, Pritchard-Jones K. Patient and public involvement to inform priorities and practice for research using existing healthcare data for children's and young people's cancers. Res Involv Engagem. 2023 Aug 29;9(1):71. doi: 0.1186/s40900-023-00485-8
2022
The Yorkshire Register is held on an encrypted firewall-protected secure platform at the University of Leeds. Individuals diagnosed with a malignant or benign central nervous system tumour aged 0–29 years whilst living in the area contiguous with the former Yorkshire and the Humber Strategic Health Authority are eligible for inclusion. Information has been collected for children diagnosed since 1974. Data accrual for 15- to 29-year-olds began in 1990.
The Yorkshire Register collects data prospectively and currently contains information on 11 702 primary and secondary tumours. Data have been linked to various administrative health-related (Hospital Episode Statistics, National Cancer Registration and Analysis Service) and non-health-related (National Pupil Database) data sets.
Personal and demographic information along with diagnostic and clinical data on treatment, death information and date last seen in follow-up clinics are available for all individuals.
Other research teams (subject to review, with the appropriate ethical and information governance approvals) can use the data held in the Yorkshire Register for the purposes of further research.
Cromie, K. J., Crump, P., Hughes, N. F., Milner, S., Greenfield, D., Jenkins, A., McNally, R., Stark, D., Stiller, C. A., Glaser, A. W., & Feltbower, R. G. 2022. Data Resource Profile: Yorkshire Specialist Register of Cancer in Children and Young People (Yorkshire Register). International Journal of Epidemiology. 13 October 2022 doi.org/10.1093/ije/dyac195
Advances in treatment and care result in the majority of children with serious diseases surviving to adulthood.1 However, many experience long-term attendant health costs. As these children move through life, it is vital to optimise their health to allow them to live the life they want and be fully participatory members of society.
The WHO defines health as a ‘state of complete physical, mental and social well-being and not merely the absence of disease or infirmity’. This demonstrates that positive social outcomes are central to good health. Governments have a responsibility to provide adequate health and social measures to achieve this.2 One key theme of the Royal College of Paediatrics and Child Health 2040 Charter is the ‘whole child approach’ emphasising the need to look beyond physical health alone.
Milner SH, Feltbower RG, Absolom KL, Glaser AW. Social outcomes after childhood illness: the missing measure.
2020
Methods: Long-term CYA survivors followed-up at a regional center in the North of England were risk-stratified by disease and treatments received into one of three levels. These data were linked with local cancer registry and administrative health data (Hospital Episode Statistics), where hospital activity was used as a marker of late morbidity burden.
Results: Poisson modelling with incident rate ratios (IRR) demonstrated similar trends in hospital activity for childhood (CH) and YA cancer survivors across NCSI risk levels. NCSI levels independently predicted long-term hospitalization risk in both CH and YA survivors. Risk of hospitalization was significantly reduced for levels 1 (CH IRR 0.32 (95% CI 0.26-0.41), YA IRR 0.06 (95% CI 0.01-0.43)) and 2; CH IRR 0.46 (95% CI 0.42-0.50), YA IRR 0.49 (95% CI 0.37-0.50)), compared with level 3.
Conclusions: The NCSI pediatric late-effects risk stratification system can be effectively and safely applied to cancer patients aged 18-29, independent of ethnicity or socioeconomic position.
Implications for cancer survivors: To enhance quality of care and resource utilization, long-term aftercare of survivors of YA cancer can and should be risk stratified through adoption of approaches such as the NCSI risk-stratification model.
Clements C, Cromie KJ, Smith L, Feltbower RG, Hughes N, Glaser AW. Risk stratification of young adult survivors of cancer to estimate hospital morbidity burden: applicability of a pediatric therapy-based approach.J Cancer Surviv 2020 (In Press) . doi:10.1007/s11764-020-00939-y.
Methods: UK treatment centres were contacted to obtain details regarding surgical interventions and long-term outcomes for patients who were treated for ALL and who developed ON in UKALL 2003 (the national leukaemia study which recruited patients aged 1 to 24 years at diagnosis of ALL between 2003 and 2011). Imaging of patients with ON affecting the femoral head was requested and was used to score all lesions, with subsequent imaging used to determine the final grade. Kaplan-Meier failure time plots were used to compare the use of CD with non surgical management.
Results: Detailed information was received for 85 patients who had developed ON during the course of their ALL treatment. A total of 206 joints were affected by ON. Of all joints affected by ON, 21% required arthroplasty, and 43% of all hips affected went on to be replaced. CD was performed in 30% of hips affected by ON. The majority of the hips were grade 4 or 5 at initial diagnosis of ON. There was no significant difference in time to joint collapse between those joints in which CD was performed, compared with no joint-preserving surgical intervention.
Conclusion: There is a high incidence of surgery in young people who have received treatment for ALL and who have developed ON. Our results suggest that CD of the femoral head in this group of patients does not delay or improve the rates of femoral head survival.
Amin NL, Kraft J, Fishlock A, White A, Holton C, Kinsey S, James B, Feltbower RG. Surgical management of symptomatic osteonecrosis and utility of core decompression of the femoral head in young people with acute lymphoblastic leukaemia recruited into UKALL 2003. The Bone and Joint Journal 2020 (In press). doi.org/10.1302/0301-620X.103B3.BJJ-2020-0239.R3.
Methods: Five-year survivors of cancer diagnosed aged 0-29 years between 1992-2009 in Yorkshire, UK were included. The cumulative count of all hospital admissions (including readmissions) for cardiovascular and respiratory conditions and all SMNs diagnosed up to 2015 was calculated, with death as a competing risk. Associations between treatment exposures and cumulative burden were investigated using multiple-failure time survival models.
Results: A total of 3464 5-year survivors were included with a median follow-up of 8.2 years (IQR 4-13 years). Ten-years post diagnosis, the cumulative incidence for a respiratory admission was 6.0 % (95 %CI 5.2-6.9), a cardiovascular admission was 2.0 % (95 %CI 1.5-2.5), and SMN was 1.0 % (95 % CI 0.7-1.4) with an average of 13 events per 100 survivors observed (95 %CI 11-15). The risk of experiencing multiple events was higher for those treated with chemotherapy drugs with known lung toxicity (HR = 1.35, 95 %CI 1.09-1.68).
Discussion: Survivors of childhood and young adult cancer experience a high burden of morbidity due to respiratory, cardiovascular diseases and SMNs up to 20-years post-diagnosis. Statistical methods that capture multiple morbidities and recurrent events are important when quantifying the burden of late effects in young cancer survivors.
Smith L, Glaser AW, Greenwood DC, Feltbower RG. Cumulative burden of subsequent neoplasms, cardiovascular and respiratory morbidity in young people surviving cancer. Cancer Epidemiol 2020;66:101711. doi.org/10.1016/j.canep.2020.101711.
2019
Methods and analysis: BONES is a prospective,longitudinal cohort study based at principal treatment centres around the UK. Participants are patients aged 10–24 years diagnosed with ALL or LBL under standard criteria. Assessment for osteonecrosis will be within 4 weeks of diagnosis, at the end of delayed intensification and 1, 2 and 3 years after the start of maintenance therapy. Assessment will consist of MRI scans of the lower limbs and physiotherapy assessment. Clinical and biochemical data will be collected at each of the time points. Bone mineral density data and vertebral fracture assessment using dual-energy X-ray absorptiometry will be collected at diagnosis and annually for 3 years after diagnosis of malignancy.
Ethics and dissemination: Ethical approval has been obtained through the Yorkshire and Humber Sheffield Research Ethics Committee (reference number: 16/YH/0206). Study results will be published on the study website, in peer-reviewed journals and presented at relevant conferences and via social media.
Amin NL, Kinsey S, Feltbower R, Kraft J, Whitehead E, Velangi M, James B. British OsteoNEcrosis Study (BONES) protocol: a prospective cohort study to examine the natural history of osteonecrosis in older children, teenagers and young adults with acute lymphoblastic leukaemia and lymphoblastic lymphoma. BMJ Open 2019;9:e027204. doi:10.1136/bmjopen-2018-027204.
Newton, HL, Friend, AJ, Feltbower, R, Hayden, CJ, Picton, HM and Glaser, AW. Survival from cancer in young people: An overview of late effects focusing on reproductive health. Acta Obstetricia et Gynecologica Scandinavica 2019; 98: 573-582. doi:10.1111/aogs.13584.
2018
Smith L, Glaser AW, Peckham D, Greenwood DC, Feltbower RG. Respiratory morbidity in young people surviving cancer: population-based study of hospital admissions, treatment-related risk factors and subsequent mortality. Int J Cancer 2018 https://doi.org/10.1002/ijc.32066
Smith L, Glaser AW, Kinsey SE, Greenwood DC, Chilton L, Moorman AV, Feltbower RG. Long-term survival after childhood acute lymphoblastic leukaemia: population-based trends in cure and relapse by clinical characteristics. Br J Haematol 2018; 182: 851-858 doi.org/10.1111/bjh.15424
Methods: We generated 10,000 simulated regions using the correlation structure and distributions from a United Kingdom dataset. We simulated cases using a Poisson distribution with the incidence rate set to the national average assuming the null hypothesis that only population size drives the number of cases. Selection of areas within each simulated region was based on characteristics considered responsible for elevated infection rates (population density and inward migration) and/or elevated leukemia rates. We calculated effect estimates for 10,000 simulations and compared results to corresponding observed data analyses.
Results: When the selection of areas for analysis is based on apparent clusters of childhood leukemia, biased assessments occur; the estimated 5-year incidence of childhood leukemia ranged between zero and eight per 10,000 children in contrast to the simulated two cases per 10,000 children, similar to the observed data. Performing analyses on region-wide data avoids these biases.
Conclusions: Studies using nonrandom selection to investigate the association between childhood leukemia and population mixing are likely to have generated biased findings. Future studies can avoid such bias using a region-wide analytical strategy. See video abstract at http://links.lww.com/EDE/B431.
Berrie L, Ellison GT, Norman PD, Baxter PD, Feltbower RG, Tennant PW, Gilthorpe MS. The association between childhood leukemia and population mixing: an artifact of focusing on clusters? Epidemiology 2018;30:75-82. doi: 10.1097/EDE.0000000000000921 .
Methods: We provided translated questionnaires covering key aspects of presentation and clinical management within 60 days of a confirmed cancer diagnosis, to patients 13-29 years of age inclusive, to their primary care physicians and to the cancer specialists managing their cancer. We conducted descriptive analyses of the data and also the process of study implementation.
Results: For our pilot, collecting triangulated data was feasible, but varying regulatory requirements and professional willingness to contribute data were key barriers. The time of data collection and the method for collecting symptom reports were important for timely and accurate data synthesis. Patients reported more symptoms than professionals recorded. We observed substantial variation in pathways to cancer diagnosis to explore definitively in future studies.
Conclusion: Focused research upon the mechanisms underpinning complex cancer pathways, and focusing that research upon specific cancer types within TYA may be the next key areas of study.
Smith L, Pini S, Ferrari A, Yeomanson D, Hough R, Riis Olsen P, Gofti-Laroche L, Fleming T, Elliott M, Feltbower R, Kertesz G, Stark D. Pathways to diagnosis for Teenagers and Young Adults with cancer in European nations – a pilot study. Journal of Adolescent and Young Adult Oncology 2018; 7:604-611. doi:10.1089/jayao.2018.0045.
Friend AJ, Feltbower RG, Hughes EJ, Dye KP and Glaser AW, Mental Health of Long Term Survivors of Childhood and Young Adult Cancer: A Systematic Review. International Journal of Cancer 2018;143:1279-1286. doi:10.1002/ijc.31337.
2017
Smith L, Norman P, Kapetanstrataki M, et al. Comparison of ethnic group classification using naming analysis and routinely collected data: application to cancer incidence trends in children and young people. BMJ Open 2017;7:e016332. doi: 10.1136/bmjopen-2017-016332
Level of treatment at PTC by diagnostic group and age group, Yorkshire 1998–2009
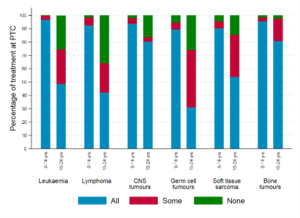
Fairley, L., Stark, D.P., Yeomanson, D. et al. Access to principal treatment centres and survival rates for children and young people with cancer in Yorkshire, UK. BMC Cancer 17, 168 (2017). doi.org/10.1186/s12885-017-3160-5
Design, setting, participants: This study assessed ON in 3113 patients aged 1–24 years who participated in the UK national leukaemia study UKALL 2003. UKALL 2003 recruited patients in 40 UK hospitals between 2003 and 2011 and included patients between ages 1 and 25 diagnosed with ALL.
Results: 170 patients were diagnosed with ON, giving a prevalence of 5.5%. The multivariable analysis showed that the risk of ON was highest for children aged between 10 and 20 years (ages 10–15 years, OR 23.7, 95% CI 14.8 to 38.0; ages 16–20 years, OR 22.5, 95% CI 12.7 to 39.8, compared with age <10 years). Among ethnic groups, Asian patients had the highest risk of ON (OR 1.92, 95% CI 1.1 to 3.6, compared with White patients). Eighty-five per cent of patients with ON had multifocal ON. Thirty-eight per cent of patients with ON required surgery and 19% of patients with ON required a hip replacement. Fifteen per cent of patients who had surgery still describe significant disability or use of a wheelchair.
Conclusions: ON has considerable morbidity for patients being treated for ALL, with a high burden of surgery. Age and ethnicity were found to be the most significant risk factors for development of ON, with Asian patients and patients aged 10–20 years at diagnosis of ALL at greatest risk. These results will help risk stratify patients at diagnosis of ALL, and help tailor future prospective studies in this area.
Amin NL, Feltbower RG, Kinsey S, et al. Osteonecrosis in patients with acute lymphoblastic leukaemia: a national questionnaire study. BMJ Paediatrics Open 2017;1:e000122. doi:10.1136/ bmjpo-2017-000122.
2016
Imam A, Fairley L, Parslow RC, Feltbower RG. Population mixing and incidence of cancers in adolescents and young adults between 1990 and 2013 in Yorkshire, UK. Cancer Causes Control. 2016;27(10):1287-1292. doi:10.1007/s10552-016-0797-3
Fairley L, Picton SV, McNally RJQ, Bailey S, McCabe MG, Feltbower RG. 2016. Incidence and survival of children and young people with central nervous system embryonal tumours in the North of England, 1990-2013. European Journal of Cancer. 61, pp. 36-43 doi:10.1016/j.ejca.2016.03.083
