The YSRCCYP provides an invaluable and unique source of data that has been used for varied research. Below is a selection from the full list of recent publications from the YSRCCYP.
2022
The Yorkshire Register is held on an encrypted firewall-protected secure platform at the University of Leeds. Individuals diagnosed with a malignant or benign central nervous system tumour aged 0–29 years whilst living in the area contiguous with the former Yorkshire and the Humber Strategic Health Authority are eligible for inclusion. Information has been collected for children diagnosed since 1974. Data accrual for 15- to 29-year-olds began in 1990.
The Yorkshire Register collects data prospectively and currently contains information on 11 702 primary and secondary tumours. Data have been linked to various administrative health-related (Hospital Episode Statistics, National Cancer Registration and Analysis Service) and non-health-related (National Pupil Database) data sets.
Personal and demographic information along with diagnostic and clinical data on treatment, death information and date last seen in follow-up clinics are available for all individuals.
Other research teams (subject to review, with the appropriate ethical and information governance approvals) can use the data held in the Yorkshire Register for the purposes of further research.
Cromie, K. J., Crump, P., Hughes, N. F., Milner, S., Greenfield, D., Jenkins, A., McNally, R., Stark, D., Stiller, C. A., Glaser, A. W., & Feltbower, R. G. 2022. Data Resource Profile: Yorkshire Specialist Register of Cancer in Children and Young People (Yorkshire Register). International Journal of Epidemiology. 13 October 2022 doi.org/10.1093/ije/dyac195
Advances in treatment and care result in the majority of children with serious diseases surviving to adulthood.1 However, many experience long-term attendant health costs. As these children move through life, it is vital to optimise their health to allow them to live the life they want and be fully participatory members of society.
The WHO defines health as a ‘state of complete physical, mental and social well-being and not merely the absence of disease or infirmity’. This demonstrates that positive social outcomes are central to good health. Governments have a responsibility to provide adequate health and social measures to achieve this.2 One key theme of the Royal College of Paediatrics and Child Health 2040 Charter is the ‘whole child approach’ emphasising the need to look beyond physical health alone.
Milner SH, Feltbower RG, Absolom KL, Glaser AW. Social outcomes after childhood illness: the missing measure.
2020
Methods: Long-term CYA survivors followed-up at a regional center in the North of England were risk-stratified by disease and treatments received into one of three levels. These data were linked with local cancer registry and administrative health data (Hospital Episode Statistics), where hospital activity was used as a marker of late morbidity burden.
Results: Poisson modelling with incident rate ratios (IRR) demonstrated similar trends in hospital activity for childhood (CH) and YA cancer survivors across NCSI risk levels. NCSI levels independently predicted long-term hospitalization risk in both CH and YA survivors. Risk of hospitalization was significantly reduced for levels 1 (CH IRR 0.32 (95% CI 0.26-0.41), YA IRR 0.06 (95% CI 0.01-0.43)) and 2; CH IRR 0.46 (95% CI 0.42-0.50), YA IRR 0.49 (95% CI 0.37-0.50)), compared with level 3.
Conclusions: The NCSI pediatric late-effects risk stratification system can be effectively and safely applied to cancer patients aged 18-29, independent of ethnicity or socioeconomic position.
Implications for cancer survivors: To enhance quality of care and resource utilization, long-term aftercare of survivors of YA cancer can and should be risk stratified through adoption of approaches such as the NCSI risk-stratification model.
Clements C, Cromie KJ, Smith L, Feltbower RG, Hughes N, Glaser AW. Risk stratification of young adult survivors of cancer to estimate hospital morbidity burden: applicability of a pediatric therapy-based approach.J Cancer Surviv 2020 (In Press) . doi:10.1007/s11764-020-00939-y.
Methods: UK treatment centres were contacted to obtain details regarding surgical interventions and long-term outcomes for patients who were treated for ALL and who developed ON in UKALL 2003 (the national leukaemia study which recruited patients aged 1 to 24 years at diagnosis of ALL between 2003 and 2011). Imaging of patients with ON affecting the femoral head was requested and was used to score all lesions, with subsequent imaging used to determine the final grade. Kaplan-Meier failure time plots were used to compare the use of CD with non surgical management.
Results: Detailed information was received for 85 patients who had developed ON during the course of their ALL treatment. A total of 206 joints were affected by ON. Of all joints affected by ON, 21% required arthroplasty, and 43% of all hips affected went on to be replaced. CD was performed in 30% of hips affected by ON. The majority of the hips were grade 4 or 5 at initial diagnosis of ON. There was no significant difference in time to joint collapse between those joints in which CD was performed, compared with no joint-preserving surgical intervention.
Conclusion: There is a high incidence of surgery in young people who have received treatment for ALL and who have developed ON. Our results suggest that CD of the femoral head in this group of patients does not delay or improve the rates of femoral head survival.
Amin NL, Kraft J, Fishlock A, White A, Holton C, Kinsey S, James B, Feltbower RG. Surgical management of symptomatic osteonecrosis and utility of core decompression of the femoral head in young people with acute lymphoblastic leukaemia recruited into UKALL 2003. The Bone and Joint Journal 2020 (In press). doi.org/10.1302/0301-620X.103B3.BJJ-2020-0239.R3.
Methods: Five-year survivors of cancer diagnosed aged 0-29 years between 1992-2009 in Yorkshire, UK were included. The cumulative count of all hospital admissions (including readmissions) for cardiovascular and respiratory conditions and all SMNs diagnosed up to 2015 was calculated, with death as a competing risk. Associations between treatment exposures and cumulative burden were investigated using multiple-failure time survival models.
Results: A total of 3464 5-year survivors were included with a median follow-up of 8.2 years (IQR 4-13 years). Ten-years post diagnosis, the cumulative incidence for a respiratory admission was 6.0 % (95 %CI 5.2-6.9), a cardiovascular admission was 2.0 % (95 %CI 1.5-2.5), and SMN was 1.0 % (95 % CI 0.7-1.4) with an average of 13 events per 100 survivors observed (95 %CI 11-15). The risk of experiencing multiple events was higher for those treated with chemotherapy drugs with known lung toxicity (HR = 1.35, 95 %CI 1.09-1.68).
Discussion: Survivors of childhood and young adult cancer experience a high burden of morbidity due to respiratory, cardiovascular diseases and SMNs up to 20-years post-diagnosis. Statistical methods that capture multiple morbidities and recurrent events are important when quantifying the burden of late effects in young cancer survivors.
Smith L, Glaser AW, Greenwood DC, Feltbower RG. Cumulative burden of subsequent neoplasms, cardiovascular and respiratory morbidity in young people surviving cancer. Cancer Epidemiol 2020;66:101711. doi.org/10.1016/j.canep.2020.101711.
2019
Methods and analysis: BONES is a prospective,longitudinal cohort study based at principal treatment centres around the UK. Participants are patients aged 10–24 years diagnosed with ALL or LBL under standard criteria. Assessment for osteonecrosis will be within 4 weeks of diagnosis, at the end of delayed intensification and 1, 2 and 3 years after the start of maintenance therapy. Assessment will consist of MRI scans of the lower limbs and physiotherapy assessment. Clinical and biochemical data will be collected at each of the time points. Bone mineral density data and vertebral fracture assessment using dual-energy X-ray absorptiometry will be collected at diagnosis and annually for 3 years after diagnosis of malignancy.
Ethics and dissemination: Ethical approval has been obtained through the Yorkshire and Humber Sheffield Research Ethics Committee (reference number: 16/YH/0206). Study results will be published on the study website, in peer-reviewed journals and presented at relevant conferences and via social media.
Amin NL, Kinsey S, Feltbower R, Kraft J, Whitehead E, Velangi M, James B. British OsteoNEcrosis Study (BONES) protocol: a prospective cohort study to examine the natural history of osteonecrosis in older children, teenagers and young adults with acute lymphoblastic leukaemia and lymphoblastic lymphoma. BMJ Open 2019;9:e027204. doi:10.1136/bmjopen-2018-027204.
Newton, HL, Friend, AJ, Feltbower, R, Hayden, CJ, Picton, HM and Glaser, AW. Survival from cancer in young people: An overview of late effects focusing on reproductive health. Acta Obstetricia et Gynecologica Scandinavica 2019; 98: 573-582. doi:10.1111/aogs.13584.
2018
Smith L, Glaser AW, Peckham D, Greenwood DC, Feltbower RG. Respiratory morbidity in young people surviving cancer: population-based study of hospital admissions, treatment-related risk factors and subsequent mortality. Int J Cancer 2018 https://doi.org/10.1002/ijc.32066
Smith L, Glaser AW, Kinsey SE, Greenwood DC, Chilton L, Moorman AV, Feltbower RG. Long-term survival after childhood acute lymphoblastic leukaemia: population-based trends in cure and relapse by clinical characteristics. Br J Haematol 2018; 182: 851-858 doi.org/10.1111/bjh.15424
Methods: We generated 10,000 simulated regions using the correlation structure and distributions from a United Kingdom dataset. We simulated cases using a Poisson distribution with the incidence rate set to the national average assuming the null hypothesis that only population size drives the number of cases. Selection of areas within each simulated region was based on characteristics considered responsible for elevated infection rates (population density and inward migration) and/or elevated leukemia rates. We calculated effect estimates for 10,000 simulations and compared results to corresponding observed data analyses.
Results: When the selection of areas for analysis is based on apparent clusters of childhood leukemia, biased assessments occur; the estimated 5-year incidence of childhood leukemia ranged between zero and eight per 10,000 children in contrast to the simulated two cases per 10,000 children, similar to the observed data. Performing analyses on region-wide data avoids these biases.
Conclusions: Studies using nonrandom selection to investigate the association between childhood leukemia and population mixing are likely to have generated biased findings. Future studies can avoid such bias using a region-wide analytical strategy. See video abstract at http://links.lww.com/EDE/B431.
Berrie L, Ellison GT, Norman PD, Baxter PD, Feltbower RG, Tennant PW, Gilthorpe MS. The association between childhood leukemia and population mixing: an artifact of focusing on clusters? Epidemiology 2018;30:75-82. doi: 10.1097/EDE.0000000000000921 .
Methods: We provided translated questionnaires covering key aspects of presentation and clinical management within 60 days of a confirmed cancer diagnosis, to patients 13-29 years of age inclusive, to their primary care physicians and to the cancer specialists managing their cancer. We conducted descriptive analyses of the data and also the process of study implementation.
Results: For our pilot, collecting triangulated data was feasible, but varying regulatory requirements and professional willingness to contribute data were key barriers. The time of data collection and the method for collecting symptom reports were important for timely and accurate data synthesis. Patients reported more symptoms than professionals recorded. We observed substantial variation in pathways to cancer diagnosis to explore definitively in future studies.
Conclusion: Focused research upon the mechanisms underpinning complex cancer pathways, and focusing that research upon specific cancer types within TYA may be the next key areas of study.
Smith L, Pini S, Ferrari A, Yeomanson D, Hough R, Riis Olsen P, Gofti-Laroche L, Fleming T, Elliott M, Feltbower R, Kertesz G, Stark D. Pathways to diagnosis for Teenagers and Young Adults with cancer in European nations – a pilot study. Journal of Adolescent and Young Adult Oncology 2018; 7:604-611. doi:10.1089/jayao.2018.0045.
Friend AJ, Feltbower RG, Hughes EJ, Dye KP and Glaser AW, Mental Health of Long Term Survivors of Childhood and Young Adult Cancer: A Systematic Review. International Journal of Cancer 2018;143:1279-1286. doi:10.1002/ijc.31337.
2017
Smith L, Norman P, Kapetanstrataki M, et al. Comparison of ethnic group classification using naming analysis and routinely collected data: application to cancer incidence trends in children and young people. BMJ Open 2017;7:e016332. doi: 10.1136/bmjopen-2017-016332
Level of treatment at PTC by diagnostic group and age group, Yorkshire 1998–2009
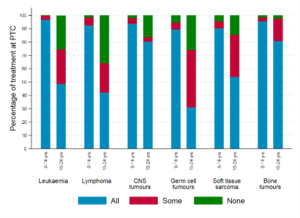
Fairley, L., Stark, D.P., Yeomanson, D. et al. Access to principal treatment centres and survival rates for children and young people with cancer in Yorkshire, UK. BMC Cancer 17, 168 (2017). doi.org/10.1186/s12885-017-3160-5
Design, setting, participants: This study assessed ON in 3113 patients aged 1–24 years who participated in the UK national leukaemia study UKALL 2003. UKALL 2003 recruited patients in 40 UK hospitals between 2003 and 2011 and included patients between ages 1 and 25 diagnosed with ALL.
Results: 170 patients were diagnosed with ON, giving a prevalence of 5.5%. The multivariable analysis showed that the risk of ON was highest for children aged between 10 and 20 years (ages 10–15 years, OR 23.7, 95% CI 14.8 to 38.0; ages 16–20 years, OR 22.5, 95% CI 12.7 to 39.8, compared with age <10 years). Among ethnic groups, Asian patients had the highest risk of ON (OR 1.92, 95% CI 1.1 to 3.6, compared with White patients). Eighty-five per cent of patients with ON had multifocal ON. Thirty-eight per cent of patients with ON required surgery and 19% of patients with ON required a hip replacement. Fifteen per cent of patients who had surgery still describe significant disability or use of a wheelchair.
Conclusions: ON has considerable morbidity for patients being treated for ALL, with a high burden of surgery. Age and ethnicity were found to be the most significant risk factors for development of ON, with Asian patients and patients aged 10–20 years at diagnosis of ALL at greatest risk. These results will help risk stratify patients at diagnosis of ALL, and help tailor future prospective studies in this area.
Amin NL, Feltbower RG, Kinsey S, et al. Osteonecrosis in patients with acute lymphoblastic leukaemia: a national questionnaire study. BMJ Paediatrics Open 2017;1:e000122. doi:10.1136/ bmjpo-2017-000122.
2016
Imam A, Fairley L, Parslow RC, Feltbower RG. Population mixing and incidence of cancers in adolescents and young adults between 1990 and 2013 in Yorkshire, UK. Cancer Causes Control. 2016;27(10):1287-1292. doi:10.1007/s10552-016-0797-3
Fairley L, Picton SV, McNally RJQ, Bailey S, McCabe MG, Feltbower RG. 2016. Incidence and survival of children and young people with central nervous system embryonal tumours in the North of England, 1990-2013. European Journal of Cancer. 61, pp. 36-43 doi:10.1016/j.ejca.2016.03.083
